Current Issue
To Establish the Effects of Being Overweight or Obese on Mental Wellbeing, Social Lives, and Education in Private Medical and Dental College Students
Irfan Ashraf1, Rizwan Azami2, Mamoona Hashim Khan3,*, Meena Hashim4, Shahida Kashif5, Zunairah Rais6, Hafiza Laila Hashim Khan7, Summera Hashim8
1Department of Anatomy and PDC, Liaquat College of Medicine & Dentistry, Karachi, Pakistan.
2Department of Surgery, Liaquat College of Medicine & Dentistry, Karachi, Pakistan.
3Final Year MBBS Student, Liaquat College of Medicine and Dentistry, Karachi, Pakistan.
4Department of Obstetrics and Gynaecology, Aga Khan University Hospital, Karachi, Pakistan.
5Department of Microbiology, Liaquat College of Medicine & Dentistry, Karachi, Pakistan.
6Department of Internal Medicine, Liaquat National Hospital, Karachi, Pakistan.
7Department of Paediatrics, Aga Khan University Hospital, Pakistan.
8Department of Paediatrics, Dow International Medical College (DIMC), Pakistan.
*Corresponding author: Mamoona Hashim Khan, Final Year MBBS Student, Liaquat College of Medicine and Dentistry, Karachi, Pakistan, Phone: +92 336 8049306, Email: [email protected]
Received Date: July 24, 2025
Publication Date: September 16, 2025
Citation: Ashraf I, et al. (2025). To Establish the Effects of Being Overweight or Obese on Mental Wellbeing, Social Lives, and Education in Private Medical and Dental College Students. Medical Research. 4(1):14.
Copyright: Ashraf I, et al. © (2025).
ABSTRACT
Background: This study aimed to investigate the prevalence of obesity and its association with mental health factors, including depression, anxiety, stress, social well-being, and mental wellness, among medical and dental students at a private college in Pakistan. Methods: A cross-sectional study was conducted among third-, fourth-, and final-year medical students of MBBS, third and final year BDS students at Liaquat College of Medicine and Dentistry over 6 months post-IRB approval. Logistic regression analyses assessed the relationships between obesity status and various mental health variables. The calculated sample size for the study was 355 participants. Data will be collected through a self-administered questionnaire. Ethical considerations involve written informed consent, ensuring data anonymity, and confidentiality. Results: The analysis revealed that students with poor social scores were 2.58 times more likely to be classified as overweight or obese compared to those with excellent scores (p=0.051). Mild stress was associated with a 60% lower likelihood of being overweight or obese (p=0.023). Students with mild anxiety were 47% less likely to be overweight or obese (p=0.026), while those with mild depression were 70.9% more likely to be classified as such (p=0.036). The type of medical educational program (MBBS vs. BDS) did not significantly influence the likelihood of obesity among students. Conclusion: The study highlights the complex relationships between mental health factors and obesity among medical and dental students. While mild stress and anxiety appear to be protective against obesity, mild depression is associated with an increased likelihood of being overweight or obese. Implementing targeted mental health support programs and promoting overall mental well-being may help improve both the mental and physical health of students in this population.
Keywords: Overweight, Obese, Mental Wellbeing, Social Lives, Medical And Dental College, Education.
INTRODUCTION
As lifestyles become more sedentary and overuse of gadgets increases, Obesity is a global problem, a lot of health problems and many physical & psychological diseases emerge. It is hypothesized that Obesity is one of them—the mother of all diseases. According to the WHO, obesity is excessive fat accumulation that presents a health risk. A body mass index (BMI) over 25 is considered overweight, and over 30 is obese. Obesity is a global problem. More than 1.9 billion adults, aged 18 and older, are overweight. Of these, over 650 million are obese. A study from Pakistan shows the prevalence of obesity in males and females was found to be 33.66 and 39.00%, respectively [1]. Depression globally is being recognized as a major public health issue, particularly in the medical student population. It causes feelings of sadness and/or a loss of interest in activities once enjoyed, and it is generally manageable. Depression affects twice as females as many compared to males. If not promptly addressed and managed, it may affect performance, social behavior, causes disturbances insomnia or excessive sleepiness, feeling worthless, guilty, and self-harming activities. Evening preference and insufficient weekday sleep duration are associated with an increased risk for suffering from depression. A past study done in Pakistan shows depression in medical students [2]. The burden of studies, poor time management compromises opportunities for medical students to relax or perform extra-curricular activities. Studies have proven that medical students, as compared to the general population, are under a tremendous burden of work. Causative factors include many aspects like time management, peer pressure, making important career choices, and financial constraints [3]. Food usually consumed in Pakistan has high calorie content has high saturated fats, trans fatty acids, free sugar, junk food, fast food, sugared fizzy drinks, and high meat consumption. Obesity can be caused by a microbiome imbalance, hormonal imbalance, a lack of sports, or no regular exercise. All these factors lead to obesity, which is causing several serious health problems like diabetes mellitus (DM), hypertension (HTN), stroke, cancer, gastroesophageal reflux, sleep apnea, osteoarthritis, polycystic ovarian disease, and many types of malignancies [4]. Medical and dental students are a particularly important group to study, as they face unique challenges such as academic stress, irregular eating patterns, and sedentary lifestyles. Despite their medical knowledge, they remain vulnerable to obesity and its psychological consequences, making them a high-risk yet understudied population. Anxiety is a feeling that is typified by anxious thoughts, bodily symptoms like elevated blood pressure, and a long-term, future-focused reaction that is primarily focused on a diffuse threat. One of the most challenging times of a person's life is the transition from adolescent to maturity that medical college students are going through. Using a variety of tools, numerous studies have documented high levels of psychological distress among medical students [5]. Both retrospective and prospective research studies have shown that most adult mental disorders begin in childhood and adolescence, which leads to obesity, depression, and anxiety. This not only impacts the personal lives but also must be affecting the quality of patient care, decision-making during emergencies, and policy-making capability of the health care system of the country. This is of immense importance especially in underdeveloped countries like Pakistan where we have a much lower literacy rate [6]. Due to maladjustment, anxiety, and despair, a large number of students in Pakistan drop out of college before completing their studies. Individuals with these disorders experience significant impacts on their social lives. Social interaction contributes to robust social networks, enhanced longevity, improved motor skills, and better memory retention. Genuine friendships foster academic success, shape personality and character, and help manage depression and anxiety, promoting overall health. Social engagement is essential for a fulfilling existence and positive well-being. This helps in the development of a healthy lifestyle, along with education [7]. Studies done in Sudan show the prevalence of obesity among students was 6.5%, and overweight was 22.2% [8]. Another study conducted in Bangladesh showed the prevalence of obesity, moderate to severe depression, and anxiety was 5.0%, 30.5%, and 16.4%, respectively, among medical students [9]. According to the narrative evaluation, at King Abdulaziz University in Jeddah, Saudi Arabia, the prevalence of depression and anxiety is very high. The incidence of depression ranged from 1.4% to 73.5%, and the incidence of anxiety ranged from 7.7% to 65.5% among medical students. Additionally, because academic standards and student life vary from one school to the next, the prevalence of depression and anxiety among medical students varies over the academic year [10]. The prevalence of overweight and obesity in medical students was found to be 36.8 % (184) and 11.1 % (55), respectively, in India [11,12]. Unlike studies conducted in the general population, the present research focuses specifically on medical and dental students in Pakistan, thereby addressing a gap in the literature. Understanding this association in future healthcare providers is significant, as it may influence both their personal well-being and their professional ability to counsel patients effectively.
MATERIALS AND METHODS
A cross-sectional study was conducted among third-, fourth-, and final-year medical students of MBBS, and third- and final-year BDS students at Liaquat College of Medicine and Dentistry over 6 months post-IRB approval (IRB Ref: [IRB/LCMD/97/2023, dated: 6th November 2023]). The sample size of 355 participants was calculated using the WHO sample size calculator, considering an expected prevalence of obesity from previous studies, 95% confidence level, and 5% margin of error. Data were collected through a self-administered questionnaire, adapted from previously validated tools and pilot-tested for clarity and reliability (Cronbach’s alpha = 0.8). Logistic regression analyses assessed the relationships between obesity status and various mental health variables. BMI was categorized according to WHO cut-offs, and mental health scores were classified using established thresholds. The regression model was specified with obesity as the independent variable and mental health outcomes as dependent variables, adjusted for age, gender, and academic year. Ethical considerations involved written informed consent, ensuring data anonymity, and confidentiality.
RESULTS
Overview of the Analysis of Social Life
The logistic regression analysis aimed to understand how social well-being, measured through a composite social score, affects the likelihood of being classified as overweight or obese among students. The social score was categorized into three levels: "Excellent," "Room for Improvement," and "Poor."
Key Results
1. Model Fit:
- The model included 355 observations.
- The Likelihood Ratio Chi-square (LR chi2) value is 5.03 with a p-value of 0.0809, indicating a marginally significant model fit. This suggests that the overall model may explain some variability in obesity status, but the p-value is above the conventional threshold (0.05), meaning we do not have strong evidence against the null hypothesis.
2. Pseudo R-squared:
- The Pseudo R² is 0.0124, indicating that the model explains only about 1.24% of the variability in the outcome variable (obesity status). This suggests that while there may be some relationship between social scores and obesity, other factors not included in the model likely play a more significant role.
3. Odds Ratios:
- The odds ratios provide insights into the likelihood of being classified as overweight or obese based on the social score categories:
- Social Score "Room for Improvement" (code 2):
- Odds Ratio: 0.812 (not statistically significant, p = 0.433)
- This indicates that students with a "Room for Improvement" social score are about 19% less likely to be overweight or obese compared to those with an "Excellent" score. However, this result is not statistically significant, meaning we cannot conclude a meaningful relationship.
- Social Score "Poor" (code 3):
- Odds Ratio: 2.583 (marginally significant, p = 0.051)
- This indicates that students with a "Poor" social score are approximately 2.58 times more likely to be classified as overweight or obese compared to those with an "Excellent" score. The p-value is very close to the 0.05 threshold, suggesting that this result may be worth further investigation.
- Social Score "Room for Improvement" (code 2):
4. Constant (_cons):
- The constant term (odds ratio of 0.348 with a significant p-value of 0.000) suggests that when all predictors are at zero, the baseline odds of being overweight or obese are low.
Conclusion
Overall, the analysis provides some evidence that social well-being may be associated with obesity among students at the private medical college, particularly indicating that poorer social scores could increase the odds of being classified as overweight or obese. However, the low Pseudo R² and the marginal significance of the "Poor" category suggest that the relationship may not be strong or may be influenced by other unmeasured factors.
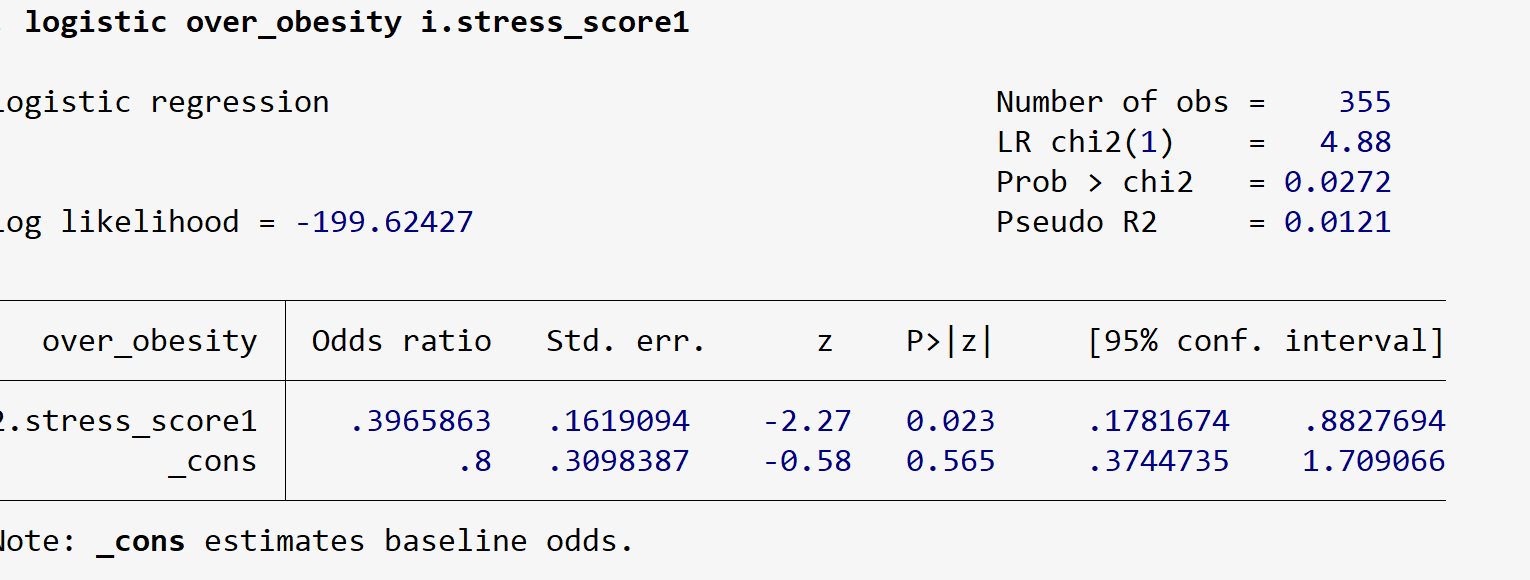
---------------------------------Stress----------------------------------------
Overview of the Analysis of stress Variables
This logistic regression aimed to assess how stress levels, categorized into different scores, affect the likelihood of being classified as overweight or obese among students at a private medical and dental college. The stress score was derived from responses to several questions about stress-related experiences.
Key intakes:
1. Model Fit: The Likelihood Ratio Chi-square (LR chi2) value is 4.88 with a p-value of 0.0272, indicating that the model is statistically significant. This suggests a meaningful relationship between stress levels and obesity status.
2. Pseudo R-squared: The Pseudo R² is 0.0121, which suggests that the model explains only about 1.21% of the variability in the obesity outcome. While the model is significant, it indicates that other factors may also play a substantial role in predicting obesity.
3. Odds Ratios: The odds ratio provides insights into the likelihood of being classified as overweight or obese based on the stress score categories:
- Stress Score "Mild" (code 2):
- Odds Ratio: 0.397 (statistically significant, p = 0.023)
- This indicates that students with mild stress are approximately 60% less likely to be classified as overweight or obese compared to those with normal stress levels. The confidence interval (0.178 to 0.883) suggests that this is a relatively strong association.
4. Constant (_cons):
- The constant term shows an odds ratio of 0.8 (not statistically significant, p = 0.565), indicating that the baseline odds of being overweight or obese when all predictors are zero are relatively low.
Conclusion
The analysis suggests that stress levels are significantly associated with obesity among students, particularly indicating that students experiencing mild stress are less likely to be classified as overweight or obese compared to those with normal stress levels. This finding could seem counterintuitive, suggesting that moderate levels of stress might be protective or that other variables influence this relationship.
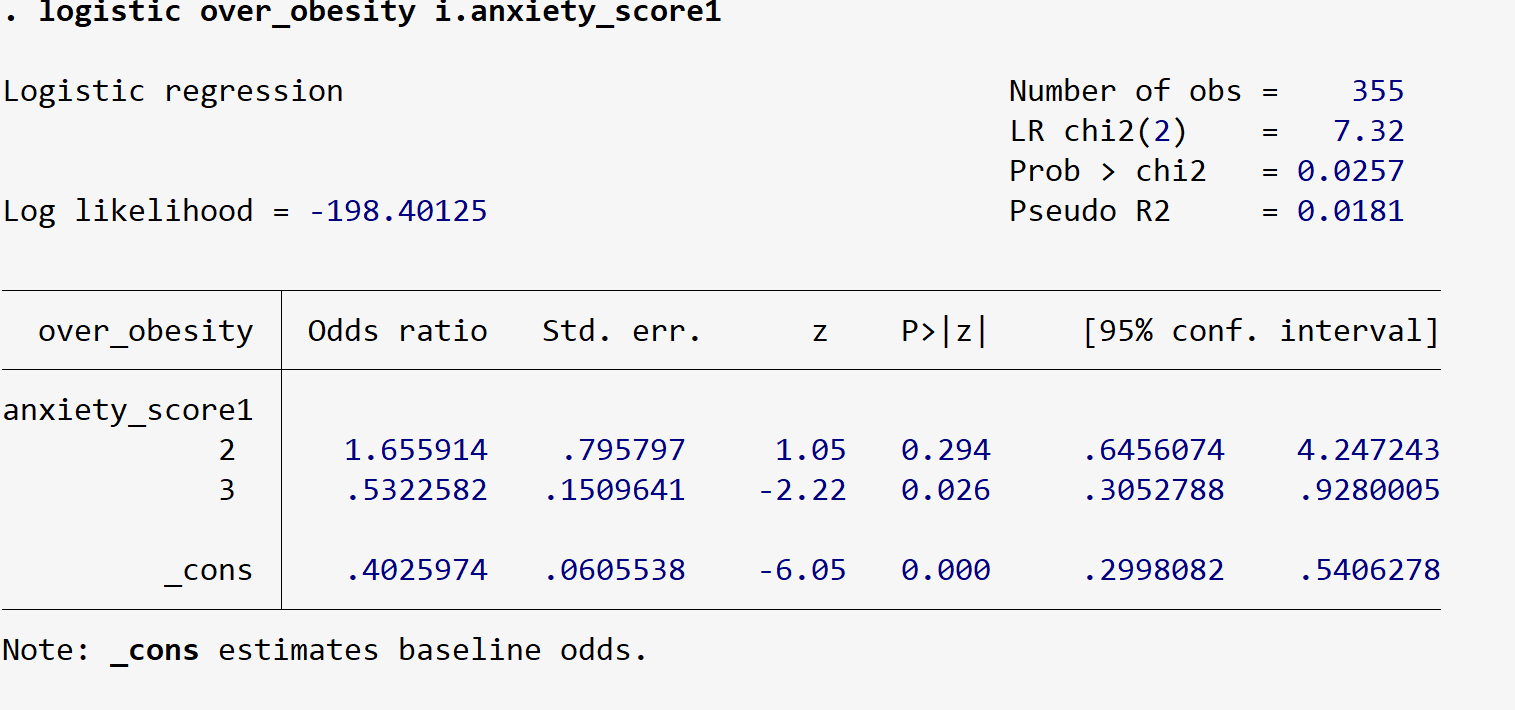
-------------------------------Anxiety Variables---------------------------------------------
Overview of the Analysis of Anxiety Variables
The logistic regression analysis aimed to determine how different levels of anxiety, measured through a composite anxiety score, influence the likelihood of being classified as overweight or obese among students at a private medical and dental college. The anxiety score was derived from responses to several anxiety-related questions.
Key Results
The Likelihood Ratio Chi-square (LR chi2) value is 7.32 with a p-value of 0.0257, indicating that the model is statistically significant. This suggests that anxiety levels have a meaningful relationship with obesity status.
1. Pseudo R-squared:
- The Pseudo R² is 0.0181, indicating that the model explains about 1.81% of the variability in the obesity outcome. While the relationship is significant, it implies that other factors likely influence obesity more substantially.
2. Odds Ratios:
- The odds ratios provide insights into the likelihood of being classified as overweight or obese based on anxiety score categories:
- Anxiety Score "Severe" (code 2):
- Odds Ratio: 1.656 (not statistically significant, p = 0.294)
- This indicates that students with severe anxiety are approximately 65.6% more likely to be classified as overweight or obese compared to those with normal anxiety levels. However, this result is not statistically significant, suggesting that we cannot draw strong conclusions from this association.
- Anxiety Score "Mild" (code 3):
- Odds Ratio: 0.532 (statistically significant, p = 0.026)
- This indicates that students with mild anxiety are approximately 47% less likely to be classified as overweight or obese compared to those with normal anxiety levels. This finding is statistically significant and suggests a protective effect of mild anxiety against obesity.
3. Constant (_cons):
- The constant term shows an odds ratio of 0.403 (highly significant, p = 0.000), indicating that when all predictors are at zero, the baseline odds of being overweight or obese are low.
Conclusion
The analysis indicates that anxiety levels are significantly associated with obesity among students. While severe anxiety does not show a strong relationship with obesity, mild anxiety appears to be protective against being classified as overweight or obese. This counterintuitive finding warrants further investigation to understand the underlying mechanisms at play.
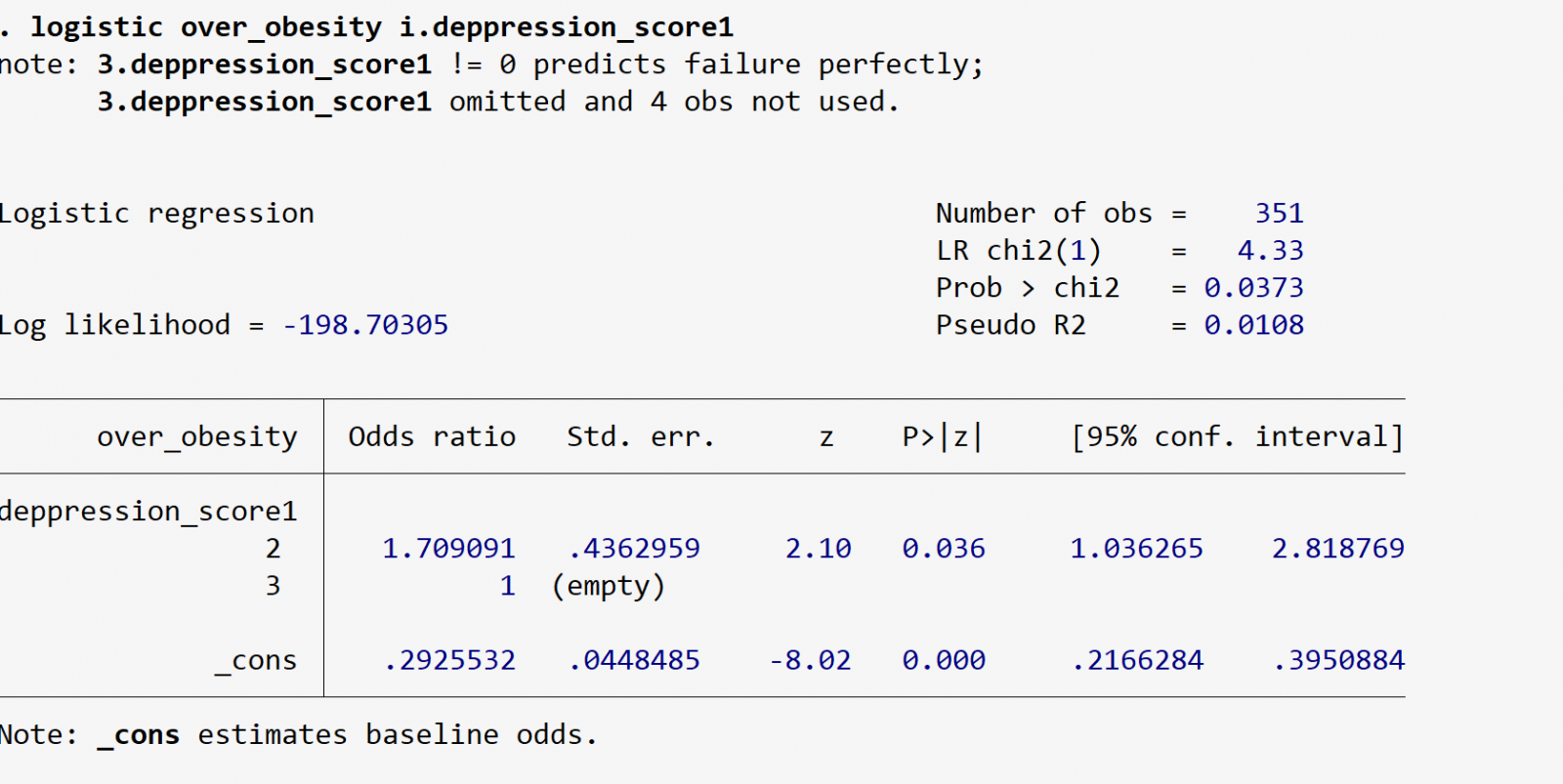
------------------------------Depression Variables----------------------
Overview of the Analysis of depression Variables
The analysis aimed to assess how different levels of depression, measured through a composite depression score, influence the likelihood of being classified as overweight or obese among students at a private medical and dental college. The depression score was calculated based on responses to various questions related to depressive symptoms.
Key Results
1. Model Fit:
- The regression includes 351 observations (four observations were omitted due to perfect prediction).
- The Likelihood Ratio Chi-square (LR chi2) value is 4.33 with a p-value of 0.0373, indicating that the model is statistically significant. This suggests a meaningful relationship between depression levels and obesity.
2. Pseudo R-squared:
- The Pseudo R² is 0.0108, indicating that the model explains about 1.08% of the variability in the obesity outcome. While significant, it suggests that other factors may play a more substantial role in obesity classification.
3. Odds Ratios:
- The odds ratios provide insights into the likelihood of being classified as overweight or obese based on depression score categories:
- Depression Score "Mild" (code 2):
- Odds Ratio: 1.709 (statistically significant, p = 0.036)
- This indicates that students with mild depression are approximately 70.9% more likely to be classified as overweight or obese compared to those with normal depression levels. This finding is statistically significant and suggests a positive association between mild depression and obesity.
- Depression Score "Severe" (code 3):
- The model omitted this category due to perfect prediction, which means that no observations were classified as "Severe." Therefore, no conclusions can be drawn about the relationship between severe depression and obesity.
- Depression Score "Mild" (code 2):
4. Constant (_cons):
- The constant term shows an odds ratio of 0.293 (highly significant, p = 0.000), indicating that when all predictors are at zero, the baseline odds of being overweight or obese are low.
Conclusion
The analysis indicates that there is a significant relationship between depression and obesity among students. Specifically, mild depression is associated with a higher likelihood of being classified as overweight or obese. However, the lack of observations in the severe depression category limits the conclusions that can be drawn about its impact.
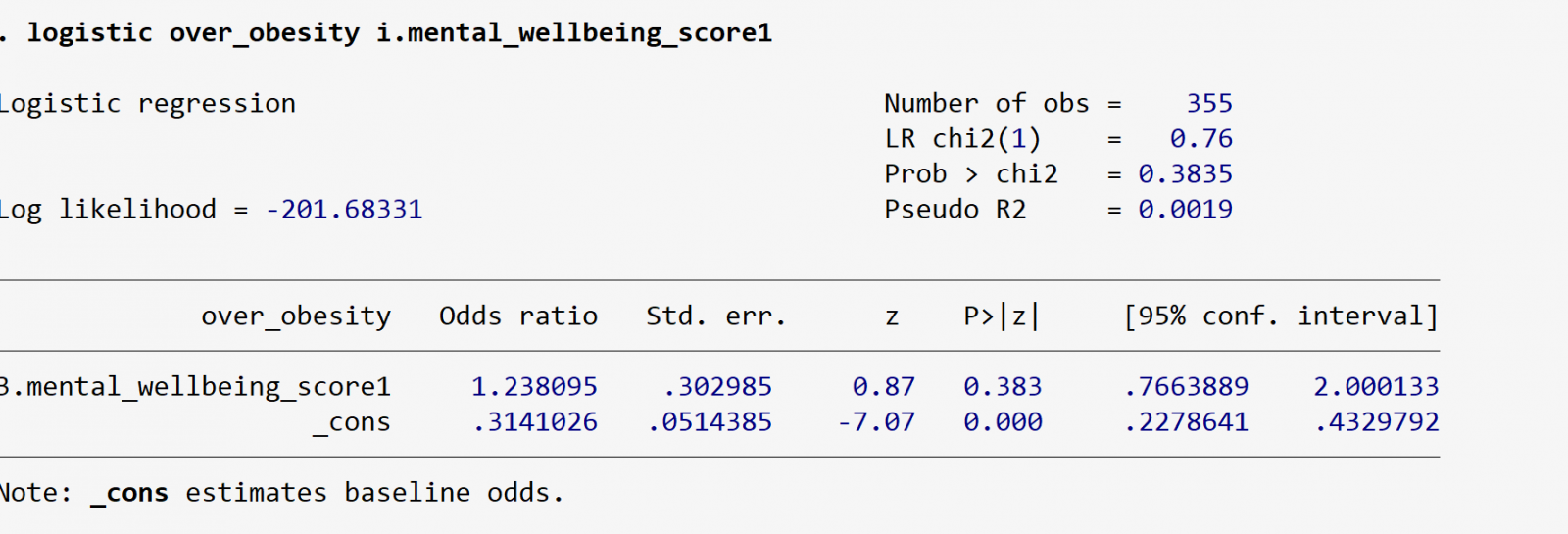
--------------------------Mental Wellness ---------------------------------------------
Overview of the Analysis of Mental Wellness
The analysis aimed to explore how different levels of mental well-being, measured through a composite score based on various positive well-being indicators, relate to the likelihood of being classified as overweight or obese among students.
Key Results
1. Model Fit:
- The regression includes 355 observations.
- The Likelihood Ratio Chi-square (LR chi2) value is 0.76 with a p-value of 0.3835, indicating that the model is not statistically significant. This suggests that the mental well-being scores do not have a meaningful relationship with obesity classification in this sample.
2. Pseudo R-squared:
- The Pseudo R² is 0.0019, indicating that the model explains a mere 0.19% of the variability in the obesity outcome. This suggests that mental well-being, as measured in this analysis, does not account for much of the variation in obesity status.
3. Odds Ratios:
- The odds ratio for the Low mental well-being category (code 3) is 1.238 (not statistically significant, p = 0.383). This implies that individuals with low mental well-being are about 23.8% more likely to be classified as overweight or obese compared to those with high mental well-being, but this finding is not statistically significant, meaning we cannot conclude that there is a true relationship based on this analysis.
4. Constant (_cons):
- The constant term shows an odds ratio of 0.314 (highly significant, p = 0.000), indicating that when all predictors are at zero, the baseline odds of being classified as overweight or obese are relatively low.
Conclusion
The analysis indicates that mental well-being, as measured through the composite score, does not significantly influence the likelihood of being classified as overweight or obese among students. The lack of statistical significance suggests that other factors may be more critical in determining obesity status in this population.
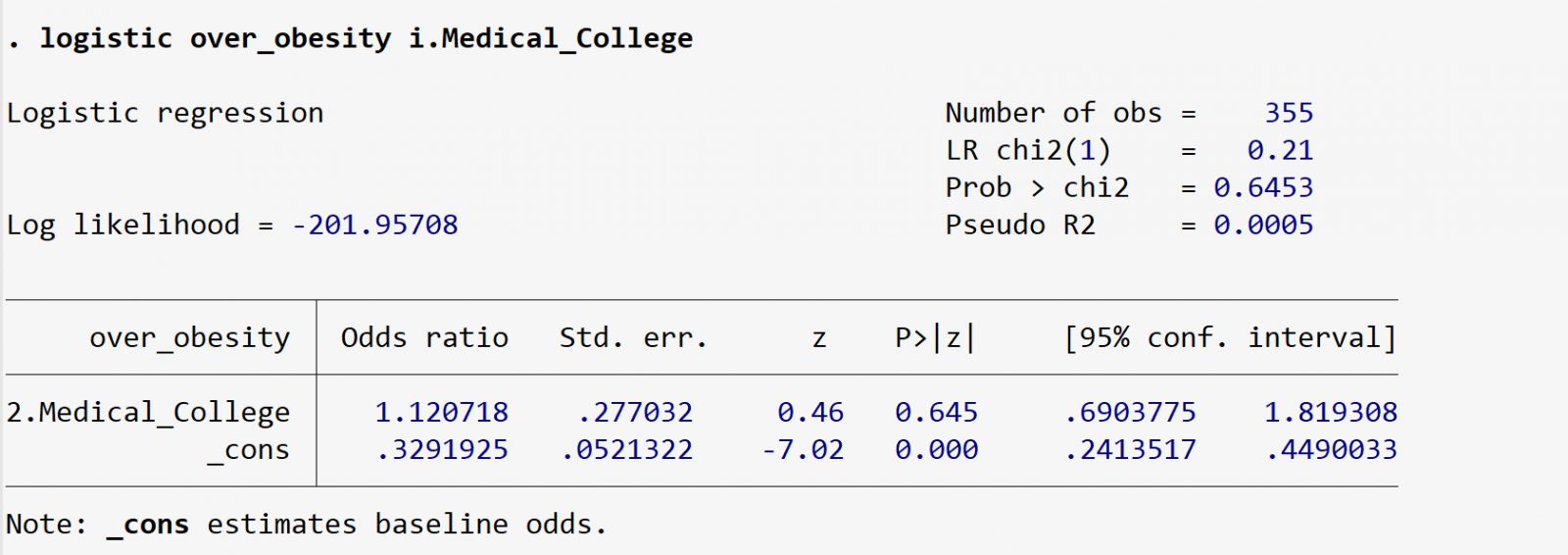
------------------------------------- Education-------------------------------------------
Analysis of Logistic Regression for Medical Educational Program and Obesity
Your analysis examines whether the type of medical educational program (MBBS vs. BDS) influences the likelihood of being classified as overweight or obese among students. Here's a detailed interpretation of your results:
Summary of Results
1. Model Fit:
- Number of Observations: The model includes 355 observations.
- Likelihood Ratio Chi-square (LR chi2): The value is 0.21 with a p-value of 0.6453. This indicates that the model does not fit the data well, and the type of medical educational program does not significantly contribute to explaining the variance in the obesity outcome.
2. Pseudo R-squared:
- The Pseudo R² is 0.0005, suggesting that only 0.05% of the variability in obesity status is explained by the type of medical educational program. This is very low, implying that other factors likely play a more significant role.
3. Odds Ratios:
- The odds ratio for the BDS program (code 2) is 1.120718. This means that students enrolled in the BDS program have about a 12% higher likelihood of being classified as overweight or obese compared to their MBBS counterparts. However, this finding is not statistically significant (p = 0.645), indicating that we cannot draw any meaningful conclusions from it.
4. Constant (_cons):
- The odds ratio for the constant term is 0.3291925, which is statistically significant (p = 0.000). This suggests that when all predictors are zero, the baseline odds of being classified as overweight or obese are relatively low.
Conclusion
The logistic regression analysis suggests that the type of medical educational program (MBBS vs. BDS) does not significantly influence the likelihood of obesity among students. The findings indicate that this variable does not explain the variation in obesity status effectively.
----------------------------------------OVERALL IMPACT------------------------------------------------
Logistic Regression Results Summary
1. Model Fit
- Number of Observations: 351
- LR chi2(6): 21.99 (p = 0.0012), indicating that at least one of the predictors is statistically significant.
- Log Likelihood: -189.87
- Pseudo R²: 0.0547, suggesting that the model explains approximately 5.47% of the variance in the likelihood of being overweight or obese.
Key Findings:
- Anxiety Score (3): Statistically significant (p = 0.001), suggesting that higher anxiety levels are associated with lower odds of being obese. This indicates that students reporting high anxiety might be less likely to be classified as obese, potentially reflecting health-conscious behaviors.
- Depression Score (2): Also statistically significant (p = 0.012), indicating that individuals with moderate depression are over 2.35 times more likely to be obese compared to those with lower depression levels.
- Other Variables:
- The coefficients for stress, anxiety (level 2), mental well-being, and the medical college program were not statistically significant, suggesting they may not have a direct effect on obesity.
Recommendations:
1. Mental Health Programs:
- Given the significant association between depression and obesity, it’s crucial to implement targeted mental health support programs. This could include counseling services, stress management workshops, and promoting awareness of mental health resources.
2. Focus on Anxiety Management:
- While anxiety levels show a complex relationship, students experiencing high anxiety should have access to relaxation and coping strategies. This could be integrated into the academic curriculum.
3. Well-being Initiatives:
- Promote overall mental well-being by organizing activities that enhance engagement and connection among students, which could positively influence their health behaviors.
Conclusion
The analysis suggests a significant relationship between mental health factors, particularly depression and anxiety, and obesity among medical students. By addressing these mental health concerns through comprehensive support systems, institutions can potentially improve both the mental and physical well-being of their students.
DISCUSSION
Compared to students who were normal weight or underweight, medical students who were overweight or obese had much inferior general health and worse body esteem. According to UK research, there was a reciprocal causal relationship between stress and emotional tiredness: high stress levels led to emotional exhaustion, and high emotional weariness led to stress. While depersonalization reduced stress levels, high degrees of personal success raised them [13]. Medical students often experience significant stress due to academic pressures, isolation is particularly pronounced during exam periods, where socializing decreases, leading to increased loneliness and emotional exhaustion [14]. In our study we have observed that there is no significant relationship between obesity and social life. The study highlighted a clear link between the year it was conducted and the rising prevalence of overweight and obesity, showing that these rates increase over time. Additionally, it was noted that male medical students exhibited a slightly higher overall prevalence of overweight and obesity than their female counterparts [14]. A study done at North Jakarta is focusing on medical students found that while anxiety is prevalent among this group, the rates of anxiety do not necessarily correlate directly with obesity. For instance, the overall prevalence of anxiety among medical students was reported at 48.9%, but this does not imply that all obese students experience high levels of anxiety [15]. We found that mild anxiety seems to be protective against being labeled overweight or obese, but severe anxiety did not exhibit a substantial correlation with obesity. Although counterintuitive, this finding is consistent with literature suggesting that in some individuals, mild anxiety may suppress appetite or increase activity levels, thereby reducing obesity risk. However, higher levels of anxiety are more often linked with disordered eating and weight gain, which may explain the absence of a simple linear relationship. Our findings indicate that moderate sadness is linked to an increased risk of being labeled overweight or obese. A cross-sectional study conducted among medical students in Peshawar highlights the broader mental health challenges faced by students, including anxiety, that often accompany depressive symptoms [16]. Previous research has highlighted the complex interplay between mental health and physical health outcomes, particularly in the context of weight status among young adults [17]. Based on the evidence, students' likelihood of being labeled overweight or obese are not substantially impacted by their mental health, as determined by the composite score. The absence of statistical significance raises the possibility that other variables may play a more important role in predicting this population's obese status here. In our study it shows BDS program (code 2) has an odds ratio of 1.120718. Thus, students in the BDS degree are around 12% more likely than their MBBS counterparts to be categorized as overweight or obese. A systematic review found that the pooled prevalence of overweight among medical students is approximately 18%, with obesity at 9% [18]. Our findings indicate in accordance with the data, there is a significant association between medical students' weight and mental health conditions, notably anxiety and sadness. Institutions may be able to enhance their students' mental and physical health by addressing these mental health issues with all-encompassing assistance networks. Study shows in universities, especially those enrolled in medical programs, frequently deal with demanding personal and academic schedules, which causes psychological stress that can result in major mental health issues like anxiety and depression [19]. Academic performance may also be impacted by the psychological toll that obesity takes. Obese students may experience stigma and bullying, which lowers their involvement in school activities and increases absenteeism. These elements may restrict future prospects and impede academic success. Taken together, our findings emphasize the need for integrated health promotion programs that combine lifestyle modification with mental health support for medical and dental students. Further longitudinal research is warranted to clarify causal pathways and to inform tailored interventions that can reduce both obesity and psychological distress in this vulnerable population [20]. At Nepal, in a cohort of 180 medical students, approximately 31.67% were classified as obese according to relative fat mass criteria. This prevalence is lower than some reports from other regions, which have documented obesity rates as high as 89% in specific populations [21]. The United States, China, India, Russia, Brazil, Mexico, Egypt, Germany, Pakistan, and Indonesia are among the ten countries with around half of the world's obese population. 17% of adults in Europe are fat, and the number of obese people is on the rise [22]. A study conducted in China evaluated the relationship between Chinese medical students' body composition and physical fitness. 2291 medical students in all were enlisted to take part in this cross-sectional investigation. They found that among medical students, a larger body mass was substantially linked to a lower level of physical fitness [23].
CONCLUSION
Given the significant association between depression and obesity, it is crucial to implement targeted mental health support programs. This could include counselling services, stress management workshops, and promoting awareness of mental health resources. While anxiety levels show a complex relationship, students experiencing high anxiety should have access to relaxation and coping strategies, which could be integrated into the academic curriculum. Institutions should consider formal policies within medical and dental education that prioritize student mental health alongside academic performance, as healthier students are more likely to become effective future healthcare providers. Furthermore, longitudinal and multi-center studies are recommended to better understand causal relationships and to guide evidence-based interventions.
AUTHOR’S CONTRIBUTION
Concept & Design of Study: MH, MNH, HLHK, SM.
Drafting: MH, MNH, HLHK, SM.
Data Collection & Analysis: MH, MNH, HLHK, SM.
Revisiting Critically: MH, MNH, HLHK, SM, IA, RA.
Final Approval of version: IA, RA.
ACKNOWLEDGEMENTS
None.
CONFLICT OF INTEREST
The study has no conflict of interest to declare by any author.
SOURCE OF FUNDING
None.
REFERENCES
- Chandio K, Shahzadi SM, Hashim H, Muhammad SD, Sumaira Talpur M, Naveel Tania. (2022). Prevalence Of Obesity AMONG MEDICAL STUDENTS OF PAKISTAN, AND ITS ASSOCIATION WITH PHYSICAL ACTIVITY AND DIETARY HABITS. Journal of Pharmaceutical Negative Results. 13(7).2411-2419.
- Asif S, Mudassar A, Shahzad TZ, Raouf M, Pervaiz T. (2020). Frequency of depression, anxiety and stress among university students. Pak J Med Sci. 36(5):971-976.
- Pathipati AS, Cassel CK. (2018). Addressing Student Burnout: What Medical Schools Can Learn From Business Schools. Acad Med. 93(11):1607-1609.
- Gazzaz ZJ, Baig M, Al Alhendi BSM, Al Suliman MMO, Al Alhendi AS, Al-Grad MSH, et al. (2018). Perceived stress, reasons for and sources of stress among medical students at Rabigh Medical College, King Abdulaziz University, Jeddah, Saudi Arabia. BMC Med Educ. 18(1):29.
- Ecker A, Berenson AB, Gonzalez SJ, Zoorob R, Hirth JM. (2022). Depression Among Medical Students in the United States During the COVID-19 Pandemic: The role of Communication Between Universities and Their Students. Disaster Med Public Health Prep. 17:e145.
- Ishii T, Tachikawa H, Shiratori Y, Hori T, Aiba M, Kuga K, et al. (2018). What kinds of factors affect the academic outcomes of university students with mental disorders? A retrospective study based on medical records. Asian J Psychiatr. 32:67-72.
- Alsubaie MM, Stain HJ, Webster LAD, Wadman R. (2019). The role of sources of social support on depression and quality of life for university students, International Journal of Adolescence and Youth. 24(4):484-496.
- Yousif MM, Kaddam LA, Humeda HS. (2019). Correlation between physical activity, eating behavior and obesity among Sudanese medical students Sudan. BMC Nutr. 5:6.
- Moonajilin S, Rahman E, Islam S. (2020). Relationship between overweight/obesity and mental health disorders among Bangladeshi adolescents: A cross-sectional survey. 18:100216.
- Mirza AA, Baig M, Beyari GM, Halawani MA, Mirza AA. (2021). Depression and Anxiety Among Medical Students: A Brief Overview. Adv Med Educ Pract. 12:393-398.
- Sonawane S, Sharma H, Tetarbe T. (2021). To study the influence of stress level with obesity in medical students of India. IP Int J Forensic Med Toxicol Sci. 6(4):153-157.
- Zafar R, Raheel M, Mujtaba MA, Mahmood R, Nawaz MU, Kumar B. (2022). Prevalence of anxiety and depression in medical students of a public sector medical college in Islamabad and coping mechanisms adopted. J Pak Med Assoc. 72(3):540-543.
- McManus IC, Winder BC, Gordon D. (2002). The causal links between stress and burnout in a longitudinal study of UK doctors. Lancet. 359(9323):2089-2090.
- Bergmann C, Muth T, Loerbroks A. (2019). Medical students' perceptions of stress due to academic studies and its interrelationships with other domains of life: a qualitative study. Med Educ Online. 24(1):1603526.
- Dewi S, Tenggara R, Hasan S. (2021). Association between stress, depression and anxiety with body fat percentage among medical students of Faculty of Medicine and Health Sciences of Atma Jaya Catholic University. Public Health and Preventive Medicine Archive. 9(1).
- Gul N, Ali A, Khan MS, Gul F, Gul A, Ali K, Haseeb SO. (2024). Prioritizing Mental Health: A Cross-Sectional Investigation of Depression Prevalence and Risk Factors among Medical Students in Peshawar, Pakistan. International Journal of Medical Students. 12(1):22-28.
- Steptoe A, Frank P. (2023). Obesity and psychological distress. Philos Trans R Soc Lond B Biol Sci. 378(1888):20220225.
- Shafiee A, Nakhaee Z, Bahri RA, Amini MJ, Salehi A, Jafarabady K, et al. (2024). Global prevalence of obesity and overweight among medical students: a systematic review and meta-analysis. BMC Public Health. 24(1):1673.
- McBeath ML, Drysdale MT, Bohn N. (2017). Pathways to mental health and wellbeing: Understanding and supporting students during critical school-to-work transitions. InWork-integrated learning in the 21st century. United Kingdom: Emerald Publishing Limited. Vol. 32. pp. 177-191.
- Sarwer DB, Polonsky HM. (2016). The Psychosocial Burden of Obesity. Endocrinol Metab Clin North Am. 45(3):677-688.
- Aryal V, Ghimire D, Kandel S, Majumder A, Manna S. (2022). Obesity among Medical Students of a Medical College: A Descriptive Cross-sectional Study. JNMA J Nepal Med Assoc. 60(255):943-946.
- Shafiee A, Nakhaee Z, Bahri RA, Amini MJ, Salehi A, Jafarabady K, et al. (2024). Global prevalence of obesity and overweight among medical students: a systematic review and meta-analysis. BMC Public Health. 24(1):1673.
- Li B, Sun L, Yu Y, Xin H, Zhang H, Liu J, Zhang Z. (2022). Associations between body composition and physical fitness among Chinese medical students: a cross-sectional study. BMC Public Health. 22(1):2041.
 Abstract
Abstract  PDF
PDF