Past Issues
Conflicts, Covid-19, and Climate Change: Challenges to Public Health in the Wake of Humanitarian Crises
Abdul Kader Mohiuddin*
Alumnus, Faculty of Pharmacy, Dhaka University, Bangladesh
*Corresponding author: Abdul Kader Mohiuddin Alumnus, Faculty of Pharmacy, Dhaka University, Bangladesh; Tel: +01706221174; Email: [email protected]
Received Date: March 9, 2023
Publication Date: March 28, 2023
Citation: Mohiuddin AK. (2023). Conflicts, Covid-19, and Climate Change: Challenges to Public Health in the Wake of Humanitarian Crises. Medical Research. 2(1):8.
Copyright: Mohiuddin AK, et al. © (2023).
ABSTRACT
Currently, humanity is facing a serious crisis. The worldwide economic contraction, the acute fall in financial asset values, the collapse in imports and exports, the contractions of industrial output, the increase in inflation, the shrinking of wages, the rise in unemployed people, and the wreckage of social security caused by numerous natural catastrophes, the human displacement due to epidemics, and ongoing rivalries tear down not only the economic sector but likewise the health sector. More than two years into the pandemic, the deadly interactions between conflicts, climate change, and COVID-19 have wreaked havoc on the food security of the most vulnerable people in the world by destroying livelihoods and raising food prices, endangering millions of people with hunger and poverty. Huge increases in food and fuel prices, as well as inflation, are all caused by conflict, the climate crisis, and COVID-19. As a result, many people are unable to afford health care.
Keywords: humanitarian crisis, shortage of medicine and medical equipment, damage to health facilities, epidemics among the refugee population
The ripple effects of war, pandemics and natural catastrophes began at a time when 1 in 16 people worldwide was just pushed into extreme poverty due to healthcare costs, 1 in 4 had already been denied access to essential medicines, and 1 in 2 lacked access to essential health services. And now, deaths due to climate shock are 30 times higher than they were 20 years ago, and hunger is killing a life every 4 seconds. Additionally, because more or less half of the world's population lacks adequate health literacy, the general public may have the hardest time understanding these issues [1].
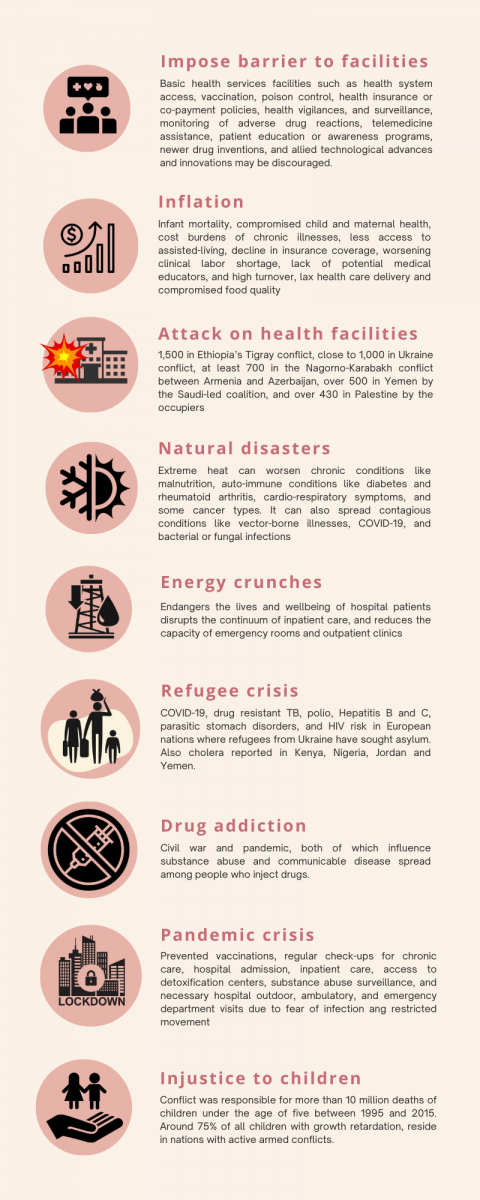
The inflation glitch included the fuel and food crises, currency devaluation, and stagflation in business, as well as 41-year highs in the US and UK; 40-year highs in Japan and Germany; 37-year highs in France and Italy; 30-year highs in India and New Zealand; and 24-year highs in South Korea, Thailand, and Turkey. Healthcare will be less concentrated if the food crisis, inflation, and economic stagflation prevail. Spending on medical and health care generally rises more quickly than overall inflation. In addition, rising inflation is associated with an increase in infant mortality; a compromise in child and maternal health; increased hospital labor expenses per patient; depression, anxiety, frustration, and stress; the cost burdens of chronic illnesses; less access to assisted-living and independent-living facilities for the elderly population; low-income households compromising food quality; a decline in insurance coverage; a worsening clinical labor shortage, a lack of potential educators, and high turnover; and lax health care delivery.
In the first ten years of the twenty-first century, wars claimed the lives of nearly 90% of civilians, many of whom were children [2]. More than 10 million deaths of children under the age of five occurred worldwide between 1995 and 2015 [3]. Conflicts also have an impact on 80% of all humanitarian needs. By 2030, up to two-thirds of the world's extremely poor people will live in unstable and conflict-ridden regions [4]. According to the 2018 World Innovation Summit for Health, 60% of chronically food insecure and malnourished people globally, including 75% of all children with stunted growth, live in conflict-affected countries [5]. Over 50 years, the Global Terrorism Database (GTD) discovered terrorist attacks in 61 different countries health facilities, with more than 50% of cases targeting medical personnel [6]. According to the WHO, 70% of all assaults on medical facilities worldwide in 2018 happened in Syria [7]. The devastation of health facilities has also been reported, including 1,500 in Ethiopia’s Tigray conflict, close to 1,000 in the Russia-Ukraine conflict, at least 700 in the Nagorno-Karabakh conflict between Armenia and Azerbaijan, over 500 in Yemen by the Saudi-led coalition, and over 430 in Palestine by the occupiers [1]. Additionally, Europe is at higher risk of COVID-19, drug-resistant TB, polio, Hepatitis B and C, parasitic stomach disorders, and HIV, which are more prevalent in European nations where refugees from Ukraine have sought asylum.
According to the UNHCR's refugee data finder, there were more than 100 million people worldwide who were displaced for various reasons, and 32.5 million people who were refugees as of mid-2022. It's also been reported that cholera is spreading among the displaced Yemeni people and Syrian refugees living in Jordan [8]. Conflict elevated the likelihood of cholera in Nigeria by 3.6 times and in the Democratic Republic of the Congo by 2.6 times, according to a recent study funded by Imperial College London [9]. Millions are being pushed into Kenya as a result of conflict, the worst drought in Somalia in 40 years, and flooding in South Sudan. In Kenya's refugee camps, cases of cholera, measles, and acute malnutrition have been documented [10]. Furthermore, half of Sub-Saharan Africa's Hepatitis E outbreaks have occurred among refugees and displaced people living in humanitarian crisis settings. Bangladesh now hosts 1.2 million refugees as a result of conflict between the Myanmar Junta and its internal rebels. In Bangladesh's Cox's Bazar refugee camp, which is the largest in the world, nearly one in eight refugees live with disabilities [11].
The pandemic started or stoked violence and conflict between countries and communities in addition to taking millions of lives. The ordinary people are the victims because the conflict was unavoidable, and there is a troubling connection between the pandemic and current political equilibrium shifts occurring around the world. The pandemic, the trade war between the United States and China, and the Ukraine crisis all threaten the global supply chain for medical equipment and raw materials. Many countries are affected by this, which is exacerbated by energy crises, freight charges, widespread disruptions in global shipping, and currency devaluations. For example, Iran has been unable to obtain essential medical supplies and life-saving medications for a long time due to various international sanctions [12 13]. The trade between India and China for medicine raw materials has been hampered due to conflicts and pandemics, or at least some trade barriers have been imposed [14-16]. Additionally, the United States may become overly dependent on Indian pharmaceutical raw materials, eliminating China as the world's most viable supplier [17-20].
A fluctuating power supply endangers the lives and wellbeing of hospital patients, disrupts the continuum of inpatient care, and reduces the capacity of emergency rooms and outpatient clinics. Uneven voltage can deteriorate thermo-sensitive supplies like vaccines, insulin, and blood transfusion products as well as biomedical machinery. According to data from Sub-Saharan Africa, power outages lasting more than 2 hours elevate mortality among inpatients above 40% [21].
Despite significant investments, over 75% of the world's emissions come from the Global North, which is causing climate events that have the greatest effects in the Global South [22]. The Institute for Economics and Peace (IEP) estimates that by 2050, conflicts and climate change may force 1.2 billion people to leave their homes [23]. Notably, since 2008, weather-related catastrophes like floods, storms, wildfires, and other extreme weather conditions have forced an average of more than 20 million people to flee their homes [24]. As a result of climate change, there are more allergenic air pollutants like mold and pollen because the warm seasons last longer. Heat waves, tropical cyclones, hurricanes, tropical storms, and flash flooding are frequent effects of extreme weather brought on by climate change. And with less precipitation, higher relative humidity, and warmer temperatures, the risk of forest fires and the ensuing air pollution will rise [25]. Extreme heat can worsen chronic conditions like malnutrition, auto-immune conditions like diabetes and rheumatoid arthritis, cardio-respiratory symptoms, and some cancer types. It can also spread contagious conditions like vector-borne illnesses, COVID-19, and bacterial or fungal infections. Agricultural workers have a 35-fold higher occupational heat-related mortality rate than workers in other industries. Cyclones, floods, and storms have caused 9 out of 10 disasters worldwide and are to blame for 3 out of 4 deaths resulting from disasters [26].
More than 50% of infectious diseases have worsened due to climate change [27]. A recent study found that despite Covid-19's continued spread, the risk of a new pandemic increases by 2% annually. Accordingly, there is a 38% chance that someone will experience a pandemic like COVID-19 in their lifetime [28]. However, more than 6.8 million people had died and 680 million had been impacted by COVID-19 as of March 7, 2023. Lockdown and the fear of being impacted have globally prevented numerous activities, including: vaccinations, regular check-ups for chronic care, hospital admission, inpatient care, access to detoxification centers, substance abuse surveillance, and necessary hospital outdoor, ambulatory, and emergency department visits. Delaying or forgoing medical care may raise the morbidity and mortality rates linked to both acute and chronic illnesses [29]. The COVID-19 pandemic alone, according to the WHO, causes a 25% increase in the prevalence of anxiety and depression worldwide [30]. Civil war and pandemic, both of which influence substance abuse and communicable disease spread among people who inject drugs (PWID).
Figure 1: Recent humanitarian crises caused by conflict, COVID-19, and climate change (Author’s own elaboration by Canva.org illustrator).
War, conflicts, climate change, and pandemics are all directly and indirectly contributing to the crisis's escalation. Surprisingly, each of these issues is linked to the others. The coexistence of all of these issues may threaten humanity by resulting in the loss of many basic health services facilities such as health system access, vaccination, poison control, health insurance or co-payment policies, health vigilances, and surveillance, monitoring of adverse drug reactions, telemedicine assistance, patient education or awareness programs, newer drug inventions, and allied technological advances and innovations. Along with access to healthcare services, technology, and innovation, the security and safety of healthcare facilities, employees, and supply lines continue to be top priorities. Any of these facilities in nations or localities would take longer to develop in a stable socio-political environment and a sound economy and would require support from the government and other allied authorities, IT innovation and protocol advancements, and public conformity to the health system. The system is extremely delicate and at risk with the variety of crises the world is currently experiencing.
REFERENCES
- Mohiuddin AK. (2023). Escalation of war and conflicts among the pandemic, natural disasters, food and economic crises: a global health concern.
- Sever FL. (2022). Wars and Children. Turkish Arch Pediatr. 57(3):253–254.
- Bendavid E, Boerma T, Akseer N, Langer A, Malembaka EB, Okiro EA, et al. (2021). The effects of armed conflict on the health of women and children. Lancet (London, England). 397(10273): 522–532.
- World Bank/International Development Association. (2022). Fragility, Conflict & Violence-Overview. World Bank.
- Gutiérrez-Romero R. (2022). Conflicts increased in Africa shortly after COVID-19 lockdowns, but welfare assistance reduced fatalities. Economic modeling. 116:105991.
- Ulmer N, Barten DG, De Cauwer H, Gaakeer MI, Klokman VW, van der Lugt M, et al. (2022). Terrorist Attacks against Hospitals: World-Wide Trends and Attack Types. Prehospital Disaster Med. 37(1):25–32.
- World Health Organization. (2018, August 19). Attacks on health care on the rise throughout Syria in first half of 2018, says WHO.
- UNICEF. (2017). From cholera in Yemen to attacks on hospitals in Syria, conflict threatens lives of over 24 million children in the Middle East and North Africa.
- Charnley GEC, Jean K, Kelman I, Gaythorpe KAM, Murray KA. (2022). Association between Conflict and Cholera in Nigeria and the Democratic Republic of the Congo. Emerg Infect Dis. 28(12):2472–2481.
- Press Release. (2022). 55 fold increase in cholera cases and an outbreak of measles in Kenya's refugee camps strain health resources, warns IRC. The International Rescue Committee (IRC).
- UNHCR. (2022). Being disabled in the world's largest refugee camp.
- Bastani P, Dehghan Z, Kashfi SM, Dorosti H, Mohammadpour M, Mehralian G. (2022). Challenge of Politico-Economic Sanctions on Pharmaceutical Procurement in Iran: A Qualitative Study. Iranian J Medical Sci. 47(2):152–161.
- Asadi-Pooya AA, Nazari M, Damabi NM. (2022). Effects of the international economic sanctions on access to medicine of the Iranian people: A systematic review. J Clin Pharm Ther. 47(12):1945–1951.
- Chaudhuri S. (2021). India's import dependence on China in pharmaceuticals: Status, issues and policy options. Research and Information System for Developing Countries.
- Sharma DC. (2020). India-China border standoff raises concerns on drug supplies. The Lancet. Oncol. 21(11):1408–1409.
- Farooq MS, Nazia F, Iftikhar A, Chun CT. (2022). China–India pharmaceutical industry cooperation in the context of “one belt, one road”: Opportunities, challenges, and the way forward. Asian J Comparat Politics. 8(1):331–347.
- Jimenez D. (2022). US pharmacopeia report finds high reliance on Indian manufacturers for APIs. Pharmaceutical Technology.
- Press Release. (2022). Gallagher, colleagues introduce Bill to end US dependence on Chinese-manufactured pharmaceuticals. Congressman Mike Gallagher.
- Artecona R, Jorge MF. (2021). United States supply chains resiliency: The key role Latin America and the Caribbean could play. Economic Commission for Latin America and the Caribbean (ECLAC).
- Shelley S. (2023). Taking Steps Toward Supply Chain Continuity. Pharmaceutical Technology, 47(3):45–47.
- Tsagkaris C, Laubsher L, Matiashova L, Lin LC, Isayeva A. (2023). The impact of energy shortages on health and healthcare in Europe. Health Sci Rep. 6(2):e1075.
- Allam Z, Bibri SE, Sharpe SA. (2022). The rising impacts of the covid-19 pandemic and the Russia–Ukraine war: Energy transition, climate justice, global inequality, and supply chain disruption. Resources. 11(11):99.
- Institute for Economics and Peace (IEP). (2022). Over one billion people at threat of being displaced by 2050 due to environmental change, conflict and civil unrest.
- UNHCR. (2016). Frequently asked questions on climate change and disaster displacement.
- Neira M, Erguler K, Ahmady-Birgani H, Al-Hmoud ND, Fears R, Gogos C, et al. (2023). Climate change and human health in the Eastern Mediterranean and Middle East: Literature review, research priorities and policy suggestions. Envir Res. 216(Pt 2):114537.
- Ryan B, Franklin RC, Burkle FM Jr, Aitken P, Smith E, Watt K, et al. (2015). Identifying and describing the impact of cyclone, storm and flood related disasters on treatment management, care and exacerbations of non-communicable diseases and the implications for public health. PLoS Currents.
- Mora C, McKenzie T, Gaw IM, Dean JM, von Hammerstein H, Knudson TA, et al. (2022). Over half of known human pathogenic diseases can be aggravated by climate change. Nature climate change. 12(9):869–875.
- Marani M, Katul GG, Pan WK, Parolari AJ. (2021). Intensity and frequency of extreme novel epidemics. Proc Natl Acad Sci U S A. 118(35) :e2105482118.
- Czeisler MÉ, Marynak K, Clarke KEN, Salah Z, Shakya I, Thierry JM, et al. (2020). Delay or avoidance of medical care because of COVID-19–related concerns — United States, June 2020. MMWR Morb Mortal Wkly Rep. 69(36):1250–1257.
- Brunier A, Drysdale C. (2022). Covid-19 pandemic triggers 25% increase in prevalence of anxiety and depression worldwide. World Health Organization.
 Abstract
Abstract  PDF
PDF